Pressure injuries remain one of the most painful and costly complications in senior care. But with the right prevention strategies and clinical support tools, providers can take control of risk and drive better outcomes — for both residents and caregivers.
The High Cost of Pressure Injuries
Treating a single Stage 2–4 pressure injury can cost between $44,000 and $90,000, not including penalties for quality-of-care deficiencies or extended hospitalizations¹. Beyond the financial burden, these injuries can severely impact residents’ health and comfort, increasing the risk of cellulitis, sepsis, gangrene, and death².
Despite decades of awareness and clinical training, pressure injuries remain common. Prevalence rates in skilled nursing settings average 20–30%, and more than 2.5 million patients in the U.S. are affected every year³.
But here’s the good news: up to 95% of pressure injuries are preventable⁴. A proactive, multi-pronged approach can significantly reduce risk and improve overall resident outcomes.
Root Causes and Smart Interventions
Cause #1: Prolonged Pressure on Bony Areas
Prolonged sitting or lying without repositioning compresses tissue and impairs blood flow, leading to skin breakdown — especially for areas like the heels, sacrum, coccyx, elbows, and shoulder blades.
Intervention: Pressure Redistribution Surfaces
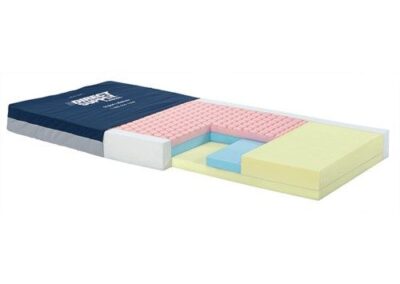
Foam and air mattresses help distribute weight across a broader surface area to reduce pressure points and are commonly used for wound prevention as well as treatment of up to Stage III wounds.
Dynamic air mattresses use alternating pressure and low-air-loss technology to shift load and manage skin moisture. These surfaces have been shown to reduce new injury occurrence by up to 45% in high-risk populations⁵.
Key stat: Foam mattresses can reduce pressure injury risk by up to 60%, compared to standard hospital mattresses⁶.
Cause #2: Microclimate and Moisture Buildup
Excess heat and moisture at the skin surface can accelerate skin breakdown.
Intervention: Skin Microclimate Management
Low-air-loss air mattresses help wick away heat and moisture.
Moisture-Wicking Fabrics: Use underpads, gowns, or linens made from fabrics designed to wick moisture away from the skin.
Breathable mattress and cushion covers improve airflow around the skin.
Gel-insert cushions help draw heat away from high-pressure areas to limit perspiration and friction-related injury.
Cause #3: Skin Shear from Friction or Movement
Sliding down in a bed or slumping in a wheelchair can cause shear forces that damage skin below the surface.
Intervention: Anti-Shear Positioning Tools
Auto-contour beds raise the knees and head simultaneously to prevent sliding.
Glide sheets, transfer boards, and low-friction fabrics reduce shear during repositioning.
Contoured cushions and lateral supports maintain better posture in seated residents.
Sleeve-style arm protectors help prevent rubbing against wheelchair parts.
Cause #4: Lack of Movement and Mobility
Limited movement causes constant pressure on vulnerable areas and slows circulation and healing.
Intervention: Repositioning, Movement & Strength Support
Specialized wheelchairs and recliners offer multiple positioning options to help redistribute pressure and reduce prolonged skin contact with high-risk areas.
Innovative wheelchair designs can also promote more independent repositioning by assisting residents into partial standing positions, giving them greater mobility and control.
Lifts and transfer devices enable safe, frequent repositioning for residents with limited mobility, reducing strain on caregivers while protecting skin integrity.
Strength and balance equipment can be incorporated into daily routines to support mobility and stamina, helping residents stay active and lowering the overall risk of pressure injuries.
Evidence-based insight: Daily mobilization has been shown to reduce pressure injury risk by up to 50%⁷.
Cause #5: Compromised Skin from Dehydration
Dehydrated skin is more fragile and prone to breakdown, especially in older adults with diminished thirst cues.
Intervention: Promote Hydration and Monitor Risk
Insulated hydration mugs and hydration carts keep fluids accessible throughout the day.
Routine vitals monitoring (including weight, temperature, and blood pressure) can help detect changes early.
One study found that in 32% of pressure injury cases, vital sign changes preceded visible skin damage⁸ — offering an early opportunity to intervene.
Pressure Injury Prevention Is Possible
Every pressure injury prevented is a win for both resident health and care team efficiency. Direct Supply offers an end-to-end suite of pressure management solutions designed specifically for senior care environments — from advanced surfaces and repositioning tools to hydration, mobility, and staff training resources.
Explore more insights or shop pressure management solutions at DirectSupply.net
Sources
¹ Hillrom Knowledge Center, 2021
² Rehabtronics White Paper on Pressure Injuries, 2021
³ AHRQ, Pressure Ulcers Overview, 2022; NPIAP 2022 Incidence Statistics
⁴ World Metrics Pressure Ulcer Statistics, 2025
⁵ World Metrics Pressure Ulcer Statistics, 2025
⁶ Cochrane Database of Systematic Reviews, 2015
⁷ BMC Nursing, 2024
⁸ Advances in Skin & Wound Care, 2021